This guide provides a clear and accessible overview of breast cancer risk factors, empowering you to take proactive steps towards your health. We’ll explore both modifiable and non-modifiable risks, offering insights into how these factors influence your individual risk profile.
Risk Factors You Can Influence
These lifestyle choices empower you to take an active role in your breast health.
- Weight Management: Maintaining a healthy weight, particularly after menopause, is crucial. Excess body fat can increase estrogen levels, potentially fueling certain types of breast cancer. A balanced diet and regular exercise are key to managing weight effectively.
- Physical Activity: Regular exercise offers numerous health benefits, including a reduced risk of breast cancer. Aim for at least 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity aerobic activity per week. Even short bursts of activity throughout the day can make a difference!
- Alcohol Consumption: Studies suggest a link between alcohol consumption and an increased risk of breast cancer. Limiting intake to one drink or less per day, or abstaining altogether, is recommended.
- Smoking Cessation: Smoking is a significant risk factor for several cancers, including breast cancer. Quitting smoking is one of the most impactful steps you can take to improve your overall health and lower your risk. Resources are available to support you in quitting.
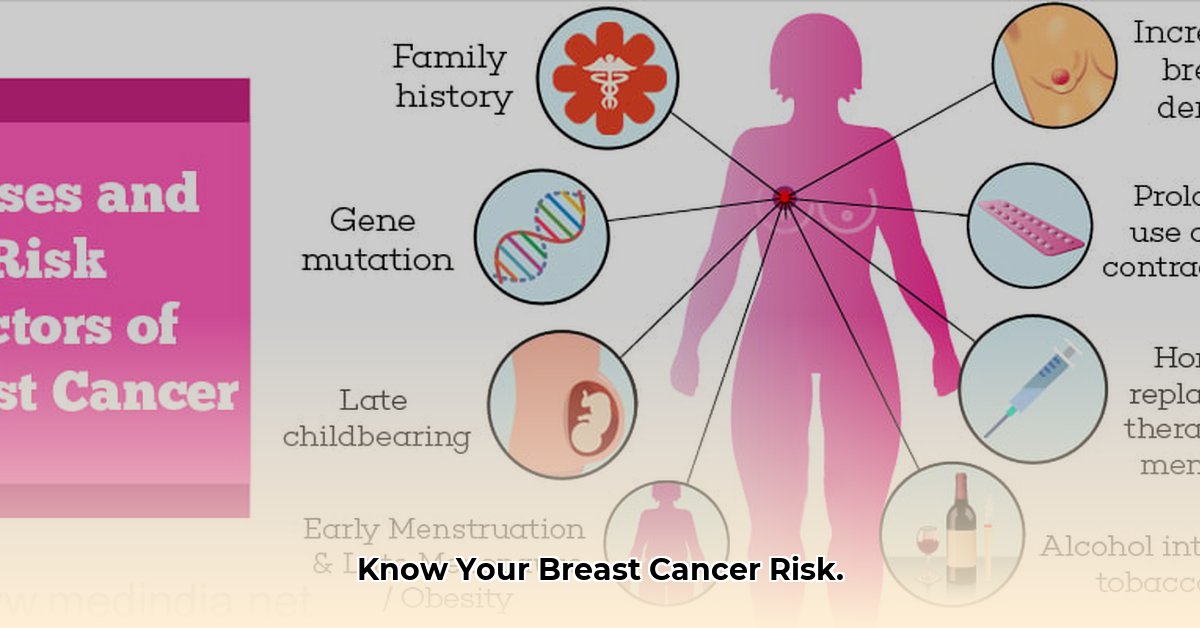
- Hormone Replacement Therapy (HRT): Combined HRT (estrogen and progestin) can slightly increase breast cancer risk. Discuss the benefits and risks with your doctor to make an informed decision about whether HRT is right for you.
- Reproductive Choices: While the impact is relatively small, having your first child after 30, not breastfeeding, or never having a full-term pregnancy may slightly increase risk. Discuss your individual circumstances with your healthcare provider.
- Night Shift Work: Some studies suggest a possible link between long-term night shift work and an increased risk of breast cancer, possibly due to hormonal disruptions. If you work night shifts, talk to your doctor about ways to minimize potential risks.
- Environmental Factors: While research is ongoing, minimizing exposure to potential carcinogens like certain pesticides and industrial pollutants may be a prudent precautionary measure.
Risk Factors You Cannot Control
Understanding these inherent risk factors allows you and your doctor to create a personalized screening and prevention plan.
- Age: The risk of breast cancer increases with age, with most diagnoses occurring after age 50. Regular screenings become increasingly important as you get older.
- Gender: Being female significantly increases breast cancer risk compared to men, largely due to hormonal differences.
- Family History: A family history of breast or ovarian cancer, particularly in close relatives (mother, sister, daughter), elevates your risk. This doesn’t mean you’ll definitely develop the disease, but it warrants discussion with your doctor and potentially genetic testing.
- Genetic Mutations: Inherited mutations in certain genes, such as BRCA1 and BRCA2, significantly increase breast cancer risk. Genetic testing can help determine if you carry these mutations, allowing for proactive management strategies.
- Race and Ethnicity: While breast cancer incidence is slightly higher in white women than Black women, Black women experience higher mortality rates. This disparity underscores the impact of socioeconomic factors and access to quality healthcare.
- Menstrual and Reproductive History: Early menstruation (before age 12) and late menopause (after 55) increase lifetime estrogen exposure, slightly raising breast cancer risk.
- Breast Density: Dense breast tissue can make mammograms more difficult to interpret and may also slightly increase risk. Discuss this with your doctor, as additional screening methods might be recommended.
- Personal History of Breast Conditions: A history of breast cancer, including DCIS (ductal carcinoma in situ) or LCIS (lobular carcinoma in situ), increases the risk of recurrence. Regular follow-up care is essential.
- Prior Chest Radiation: Radiation therapy to the chest, especially during childhood or adolescence, can increase the risk of developing breast cancer later in life.
- DES Exposure: Prenatal exposure to diethylstilbestrol (DES), a drug prescribed to some pregnant women between the 1940s and 1970s, slightly increases breast cancer risk in daughters.
- Height: Some studies suggest a correlation between height and a slightly increased risk of breast cancer, although the reasons for this are not fully understood.
Understanding Your Family History
A family history of breast cancer provides crucial insights into your personal risk. When discussing your family history with your physician, be prepared to provide information regarding:
- Which relatives have had breast cancer (mother, sister, grandmother, aunt, etc.)
- Their age at diagnosis (early-onset breast cancer, before age 50, may suggest a genetic predisposition)
- The type of breast cancer (if known)
- Whether they had ovarian cancer (as some gene mutations increase the risk of both)
Assessing Your Personal Risk
Understanding your personal risk involves considering your individual circumstances and family history. The following tools and resources can assist in this assessment:
- Breast Cancer Risk Assessment Tool (BCRAT): The National Cancer Institute (NCI) offers the BCRAT, an online tool that calculates your risk based on personal and family health information: https://www.cancer.gov/bcrisktool/
- Consult Your Doctor: Discussing your risk factors with your physician is crucial. They can help interpret your BCRAT results, answer your questions, and recommend a personalized screening and prevention plan.
Empowering Yourself Through Knowledge
Knowledge is power. Understanding your breast cancer risk factors empowers you to make proactive choices about your health. While some factors are beyond your control, adopting a healthy lifestyle and discussing your personal risk with your doctor can significantly contribute to your well-being. Remember, risk assessment tools provide probabilistic estimates, not certainties. Open communication with your healthcare provider is the best way to develop a personalized plan that addresses your unique needs. Early detection and prevention are your strongest allies.